Image-guided Radiotherapy (IGRT)
What is Image-Guided Radiation Therapy and how is it used? Who will be involved in this procedure? What equipment is used? Who operates the equipment? Is there any special preparation needed for the procedure? How is the procedure performed? What will I feel during and after this procedure?Overview
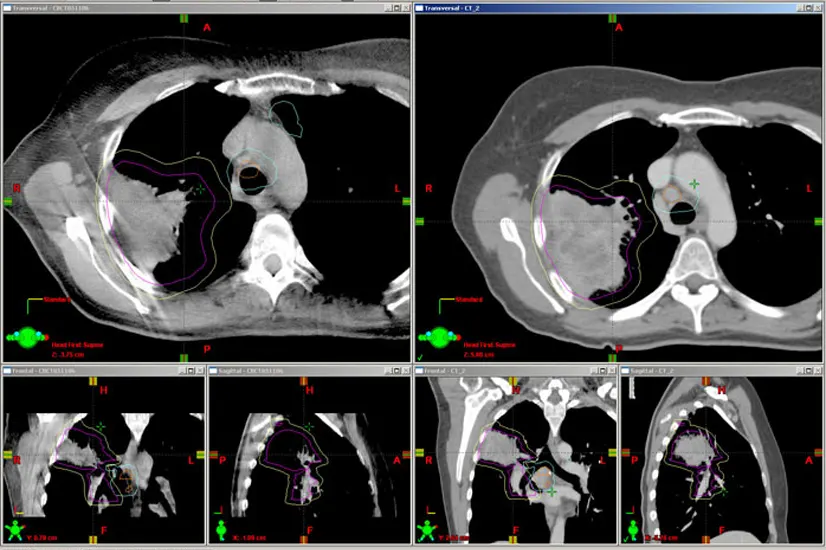
Image-guided radiation therapy (IGRT) is the use of imaging during radiation therapy to improve the precision and accuracy of treatment delivery. IGRT is used to treat tumors in areas of the body that move, such as the lungs. Radiation therapy machines are equipped with imaging technology to allow your doctor to image the tumor before and during treatment. By comparing these images to the reference images taken during simulation, the patient's position and/or the radiation beams may be adjusted to more precisely target the radiation dose to the tumor. To help align and target the radiation equipment, some IGRT procedures may use fiducial markers, ultrasound, MRI, x-ray images of bone structure, CT scan, 3-D body surface mapping, electromagnetic transponders or colored ink tattoos on the skin.
If you are to undergo IGRT, your doctor will likely use CT scanning to conduct a treatment simulation session and to create reference images. Other imaging procedures, such as MRI or PET scan, may be used to help determine the exact shape and location of your tumor, and a special device may be created to help you maintain the same exact position during each treatment. Your doctor will give you specific instructions based on the type of exam being performed.
What is Image-Guided Radiation Therapy and how is it used?
Image-guided radiation therapy (IGRT) is the use of frequent imaging during a course of radiation therapy for the purpose of improving the precision and accuracy of the delivery of radiation treatment.
In IGRT, machines that deliver radiation, such as a linear accelerator (for x-ray or photon) or cyclotron/synchrotron (for proton), are equipped with special imaging technology that allow the physician to image the tumor immediately before or even during the time radiation is delivered, while the patient is positioned on the treatment table. Using specialized computer software, these images are compared to the reference images taken during simulation. Any necessary adjustments are made to the patient's position and/or radiation beams in order to more precisely target radiation at the tumor and avoid healthy surrounding tissue.
Computed tomography (CT), magnetic resonance imaging (MRI), ultrasound (US) and x-ray imaging may be used for IGRT by visualizing bony or soft-tissue anatomy. Other methods for IGRT use markers placed on the patient's body surface or implanted within the patient's body.
IGRT is used to treat tumors in areas of the body that are prone to movement, such as the lungs (affected by breathing), liver, pancreas, and prostate gland, as well as tumors located close to critical organs and tissues. It is often used in conjunction with intensity-modulated radiation therapy (IMRT), proton beam therapy, stereotactic radiosurgery, or stereotactic body radiotherapy (SBRT), which are advanced modes of high-precision radiotherapy that utilize computer-controlled x-ray accelerators to deliver precise radiation doses to a malignant tumor or specific areas within the tumor. See the IMRT page, Proton Beam Therapy page or SBRT page for more information.
Who will be involved in this procedure?
Delivery of radiation therapy requires a treatment team, including a radiation oncologist, therapeutic medical physicist, dosimetrist and radiation therapists. The radiation oncologist is a physician who evaluates the patient and determines the appropriate therapy or combination of therapies and the type of IGRT. The physician determines what area to treat and what dose to deliver. Together with the therapeutic medical physicist and the dosimetrist, the radiation oncologist determines what techniques to use to deliver the prescribed dose. The physicist and the dosimetrist then make detailed treatment calculations. Radiation therapists are specially trained technologists who acquire images and deliver the daily treatments. The radiation oncology nurse assesses the patient and provides the patient with additional information about the treatment and possible adverse reactions. The radiation oncology nurse also helps manage any reactions or side effects from treatment that may occur, in collaboration with the physician.
What equipment is used?
In IGRT, imaging equipment is mounted on or built into the machine that delivers radiation, such as a linear accelerator. Imaging equipment may also be mounted in the treatment room. Imaging technologies used in IGRT include x-rays, computed tomography (CT), 3-D body surface mapping, magnetic resonance imaging (MRI) and ultrasound (US). Sometimes, IGRT is performed by a detector in the room which tracks motion by localizing markers on the surface of a patient, or electromagnetic transponders placed within the patient
Who operates the equipment?
The equipment is operated by a radiation therapist, a highly trained technologist. The overall treatment plan is created and supervised by the radiation oncologist, a highly trained physician specializing in treating cancer with radiotherapy.
Is there any special preparation needed for the procedure?
Women should always inform their physician or technologist if there is any possibility that they are pregnant or if they are breastfeeding their baby. See the Safety page for more information about pregnancy, breastfeeding and imaging. Patients with pacemakers or loose metal in their bodies should inform the treatment team if MRI is used for simulation or IGRT.
For some IGRT procedures, very small markers, which are called fiducial markers, or in some cases electromagnetic transponders may be placed inside the body near or in the tumor to help the treatment team identify the area. They are usually placed at least one week prior to the first radiation therapy treatment. The patient's skin also may be marked or tattooed with colored ink to help align and target the radiation equipment. Patients with prostate cancer who undergo IGRT using ultrasound must drink enough water about an hour before each treatment to keep their bladder full so that the prostate can be imaged or "seen" by the ultrasound machine. See the Fiducial Marker Placement page for more information.
Otherwise, there is no specific preparation for IGRT, other than the preparation for routine radiation therapy, which could be either 3-D conformal radiation therapy, intensity modulated radiation therapy (IMRT), proton beam therapy, or stereotactic body radiotherapy (SBRT). See the IMRT page, Proton Beam Therapy page or SBRT page for more information.
How is the procedure performed?
At the beginning of each radiation therapy session, the patient is carefully positioned guided by the marks on the skin defining the treatment area. Devices may be used to help the patient maintain the proper position. Images are then taken using imaging equipment that is built into the radiation delivery machine or mounted in the treatment room.
Some IGRT techniques require patients to hold their breath for approximately 30 to 60 seconds. If IGRT requires fiducial markers or electromagnetic transponders inside the body, these will be inserted into the body with a needle about a week prior to the simulation process.
On each treatment day, depending on the type of IGRT used, an x-ray, CT scan or ultrasound will be obtained prior to the treatment. The physicians or a radiation therapist review the images and compare them to the reference images taken during simulation to make position adjustments. The patient may be repositioned and additional imaging may be performed. After any necessary adjustments are made to match with the patient's reference positioning, radiation therapy is delivered.
The image-guidance process is expected to add additional time to each radiation therapy session.
What will I feel during and after this procedure?
Imaging performed prior to or during radiation therapy sessions is painless.
During the radiation therapy session, you may see or hear equipment moving around you during the imaging procedure. Patients may sometimes smell an odd smell during treatment that is caused by the ozone produced by the linear accelerator. Some patients may also see a colored light when they receive their treatment; this event is especially true for patients having their brain treated.
Radiation treatment can cause side effects. These problems may result from the treatment itself or from radiation damage to healthy cells in the treatment area.
The number and severity of side effects will depend on the type of radiation, dose, and body part under treatment. Talk to your doctor and/or nurse so they can help manage them.
Radiation can cause early and late side effects. Early side effects happen during or right after treatment. They are typically gone within a few weeks. Common early side effects include fatigue and skin problems. Skin in the treatment area may become sensitive, red, irritated, or swollen. Other changes include dryness, itching, peeling, and blistering.
Depending on the area being treated, other early side effects may include:
- hair loss in the treatment area
- mouth problems and difficulty swallowing
- eating and digestion problems
- diarrhea
- nausea and vomiting
- headaches
- soreness and swelling in the treatment area
- urinary and bladder changes
Late side effects may occur months or years following treatment. While they are often permanent, they are rare. They include:
- brain changes
- spinal cord changes
- lung changes
- kidney changes
- colon and rectal changes
- infertility
- joint changes
- lymphedema
- mouth changes
- secondary cancer
There is a slight risk of developing cancer from radiation therapy. After treatment, your radiation oncologist will regularly check for complications and recurrent or new cancers.
Using techniques such as IGRT, imaging specialists are maximizing the cancer-destroying capabilities of radiation treatment while minimizing its effect on healthy tissues and organs and the side effects of the treatment itself.